Project Data
Tel Aviv, Israel
Location
Ranni Ziss Architects and Sharon Architects
Architects
Tel Aviv Sourasky Medical Center in Israel
Client
70,000 m2 (753,500 sq. ft.)
Building area
Design started in 2005. Primary system constructed in 2008 – 2011; Secondary and Tertiary systems ongoing construction from 2008.
Design/Construction
Structural grid of 7.6 x 7.6 m (25 x 25 ft), central core of elevators and stairs, distributed MEP shafts, and the building envelope.
Primary System
Non-loadbearing walls and MEP systems.
Secondary System
Ward equipment, including medical devices, digital tech, and furniture.
Tertiary System
Dr. Nirit Pilosof
Case Study report
Introduction
The case of the Sammy Ofer Heart Building at Tel Aviv Sourasky Medical Center demonstrates the contribution of the Open Building approach to the evolutionary process of a healthcare building over time. While most hospital facilities are “tailor-made” - designed for a highly detailed functional program, the design team of the Sammy Ofer Heart Building challenged this traditional practice and proposed a flexible design for unknown future functions (Pilosof, 2020; Sharon, 2012). To maximize the value of a private donation and expand the hospital capacity to evolve in the future, the hospital CEO decided to defer the decision on the uses of seven of its eleven floors for later consideration. Accordingly, the need to design a Base Building as a “container with capacity” that could accommodate unknown functional programs led to the implementation of system separation (Figure 4). Although the open building approach (Kendall, 2008) was not explicitly stated by anyone in the design process, its methods of system separation and distributed design management implicitly supported the construction of the project in phases, enabled the design of a variety of changing functional spaces, and enhanced the management and coordination of the design process by different consultants, designers and contractors.
The design process
The project was designed by Sharon Architects and Ranni Ziss Architects, a joint venture, and was developed starting in 2005 and constructed in 2008 - 2011. The building, located in the center of Tel Aviv, was designed as a monolithic cube clad in glass with prominent red recessed balconies. The building was designed to connect to an adjacent, historical ‘Bauhaus’ hospital building through an atrium with iconic red recessed balconies (Figure 1). The 70m (230ft.) high building consists of 55,000 m2 (592,000 sq. ft.) and includes 13 medical floors of 3,100 m2 (33,300 sq. ft.) per floor, and four underground parking floors designed with the possibility of conversion to an emergency 650-bed hospital. The 15,000 m2 (161,400 sq. ft.) underground “sheltered” floors were designed in an innovative way to be resistant to chemical and biological warfare.
The main force behind the design and construction of the building was the generous donation of the Sammy Ofer family to the Tel Aviv Sourasky Medical Center in 2005. Since hospital development in Israel relies primarily on private funding, hospital directors attempt to maximize the potential of each donation. In the case of Tel Aviv Sourasky Medical Center, it was clear from the start that the hospital would construct the most extensive structure possible even by applying pressure on the municipality planning guideline limitations (Figure 3). This strategy led to the design of a base building with seven shell floors for future completion, and was even more evident in the ‘last minute’ decision to add two more shell floors to the building just before construction began. This change of the buildings’ height required redesigning the buildings’ primary system, including the structure, MEP systems and facades and caused a delay of a few months in the design and construction process. In 2022, a decade after the building was opened, the hospital management decided to add three more floors to the top of the existing building to offer more space in the highly dense urban site. (Figure 3)
The project was programmed and designed by the architects in collaboration with the hospital CEO, deputy director, head of cardiology units, head nurse, and various internal and external consultants and project managers. Like most hospital facilities, the project was planned under tight budgetary, regulatory and environmental constraints. The design process, which began in 2005, reflected a variety of concepts. The realization of the project depended on finding a solution for an existing (but now obsolete) two-story outpatient building that had been constructed on the site in the 1960s for use as an emergency department. After much discussion, that building was demolished. Because the hospital management was undecided regarding their strategy and program, the design team developed a method of presenting and evaluating diverse design options for the new project.
The building, defined as a cardiac care center, was initially programmed to relocate all the hospital cardiac units, clinics, and surgery division onto three main floors and include an additional two floors for internal medicine units and outpatient clinics. Seven additional floors were also built but left empty for future programming and Infill or fit-out. Accordingly, the new building was constructed in five main phases: (1) the underground emergency hospital, (2) core and envelope (Base Building) of floors 1-10 including a mechanical roof floor, (3) interior fit-out of floors 0-3, (4) interior fit-out of floors 4-6, and (5) interior fit-out of floors 7-10. The hospital plans to construct three additional floors on top of the existing building in 2023, adding 8,500 m2 (91,500 sq. ft) for diverse inpatient and outpatient units (Figure 3).
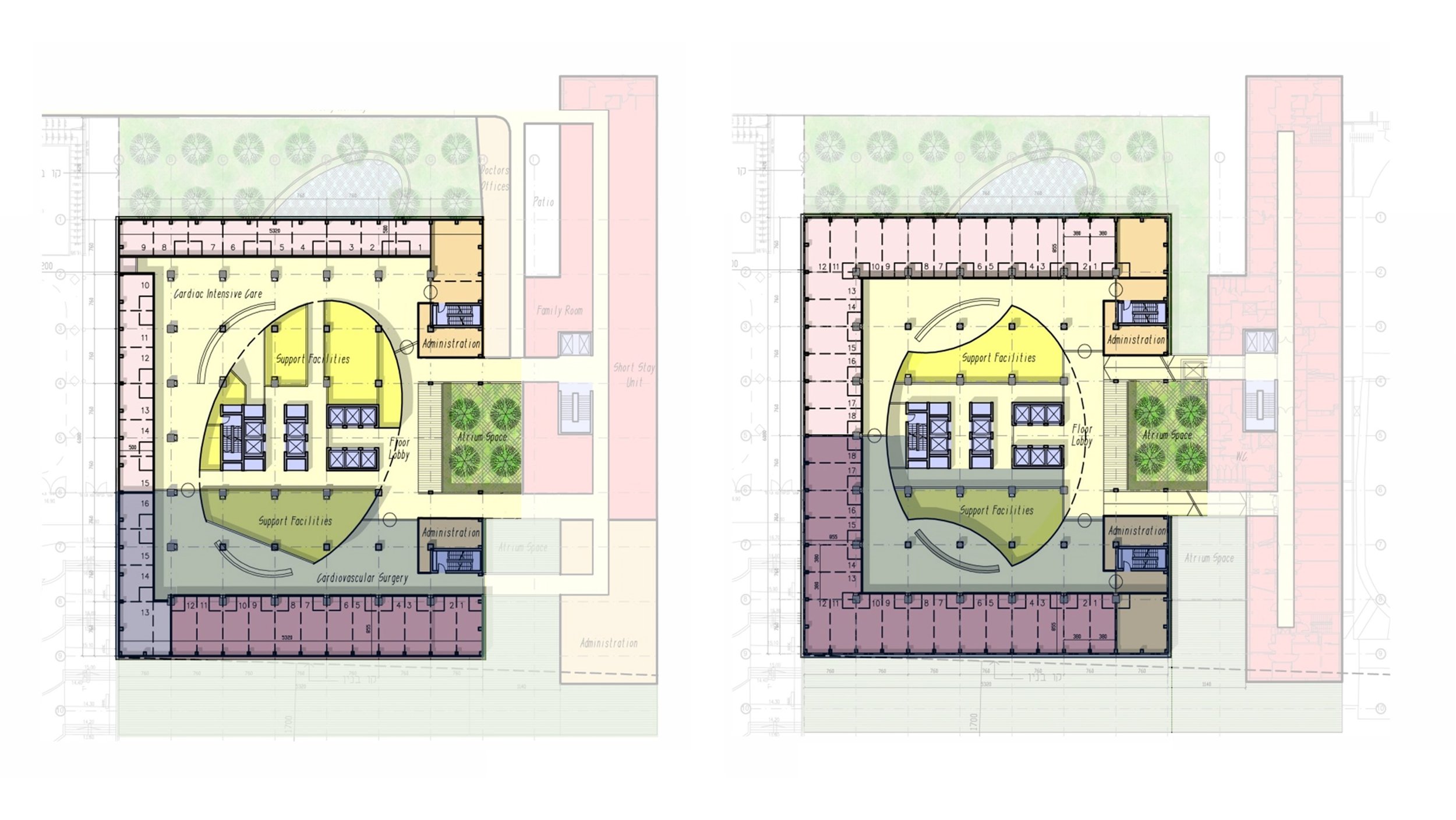
The design process from the beginning included capacity studies to analyze if the primary system could accommodate the predicted development of the building in the future as defined by the hospital CEO and medical directors. The preliminary studies included schematic drawings of a typical floor with two inpatient medical units to illustrate the capacity for both: two identical mirrored units vs one major unit with more ICU rooms and a minor unit with semi-private rooms (Figure 2). The client also required the architects to prepare a schematic design for the research lab and Neurology units that were expected to be installed in the shell (empty) floors of the building. The primary purpose of the capacity studies was to analyze if the primary system (Base Building) would support future anticipated programs, the location of heavy equipment, possible connections to MEP infrastructures and efficient configuration of functions. Research on the evolutionary process of the building over thirteen years revealed that the preliminary capacity analysis study drawings were retained and were later used to evaluate the potential of the building for future change and to analyze the interfaces between the different system levels (Pilosof, 2018). In this sense, these drawings became a communication tool between the initial design team and the following design teams, their importance unknown at the time of the initial design, to demonstrate the open building approach (which at that time had no formal name to the design team or client) and to explain the decision making throughout the design.
The evolution of the building
The Sammy Ofer Heart Building, defined and designed as a cardiology center, has changed its functional program considerably. The cardiology division in fact, occupies less than 30% of the building. The building now contains neurology, dermatology, internal medicine and oncology units in addition to research labs and outpatient clinics (Figures 3 and 4). The change of program can be explained by changing needs since cancer became the number one cause of death and statistically surpassed cardiac diseases. The logic of centralizing the oncology units in one location to enhance the hospital efficiency and health services could only have been accomplished in the new building. The hospital management also decided to relocate other functions to the building since their previous locations required renovation or extension or received funds to reconstruct a specific medical unit. In some cases, the decision to relocate medical units to the new building was the result of competition with other hospitals, or a strategy to attract highly accomplished medical directors. Throughout the years, the hospital’s dynamic development plan has been driven by forces of economics as well as internal and external organizational politics.
Most of the changes took place after the building was occupied. Although this process of deferred completion of secondary and tertiary systems was planned in advance, it still created a challenge both for the construction and the operation of the running units. The phasing stages, divided by the buildings’ floors, created a fit-out process from the bottom upwards. This strategy might be efficient in order to avoid interruptions of the completion to the operating units, but it limits decision- flexibility during the design process. In many cases the considerations in the fit-out installation phases overruled the importance of locating some medical functions close to other units for process optimization. For example, the inpatient internal medicine units under construction on the 9th floor should have been located on the 4th floor above the existing internal medical units (on the 3rd floor) to centralize the internal medicine division and enhance staff and equipment flows among the four units.
The separation of the building into system levels was also useful as a project management and budgeting tool in the design process. The long design process of thirteen years, which was still running in 2018, involved many different professionals and decision makers. Many of the project team members of the hospital were replaced, including the CEO of the hospital, heads of medical units and head nurses. Each change of personnel resulted in reconsideration of the design and requests for alternative design options. The design team included a collaboration of two architecture firms, the replacement of two project management firms, and consultants who changed over time. The development of the project by phases, using system levels, allowed the architects to divide the workload between the two offices. Each office was responsible for designing specific floors’ secondary systems, with minimal need for consultation and coordination. The design control was distributed between the two firms on each level (e.g. the primary, secondary and tertiary system levels) to avoid inequal division between the two firms. The study also indicates that capacity study drawings that were developed at a preliminary stage were used as communication tools later, among design teams not even known initially, because they defined the anticipated interfaces between the system levels. The recent decision to add three floors to the top of the building demonstrates the capacity of the original design to grow even beyond its initial build-out. It highlights the unpredictability of future needs and the necessity to plan for change over time.
Acknowledgments
This research was supported by the European Research Council grant (FP-7 ADG 340753), and by the Azrieli Foundation. I am grateful to the Tel Aviv Sourasky Medical Center management and staff, and to Ranni Ziss Architects, Sharon Architects, CPM and M. Iuclea project managers for their collaboration.
References
Pilosof, N. P. (2018). The evolution of a hospital planned for change. In S. H. Kendall (Ed.), Healthcare Architecture as Infrastructure (pp. 91–107). Routledge.
Pilosof, N. P. (2020). Building for Change: Comparative Case Study of Hospital Architecture. HERD: Health Environments Research & Design Journal, 193758672092702. https://doi.org/10.1177/1937586720927026
Sharon, A. (2012). Flexible building design offers future-proofing. IFHE DIGEST, 96–98.